Denver was recently the focal point of groundbreaking HIV research, hosting the esteemed Conference on Opportunistic Infections and Retroviruses (CROI). This annual event, attended by over 5000 experts, showcased the latest scientific findings, with this year’s spotlight on the critical intersection of HIV and noncommunicable diseases (NCDs), particularly cardiovascular conditions.
Leading the charge, Lily D. Yan from Weill Cornell Medicine presented a pioneering study focused on treating prehypertension in people living with HIV (PLWH). Their randomized controlled trial with 250 participants in Haiti revealed that initiating antihypertensive treatment at lower blood pressure thresholds significantly reduces both blood pressure and the incidence of hypertension, with minimal side effects, underscoring the need for revised treatment guidelines in PLWH to reduce incidents of severe cardiovascular events.
Chris Longenecker from the University of Washington (and MPI of HLB-SIMPLe’s PULESA project) reported on the EXTRA-CVD trial. The EXTRA-CVD team tested a nurse-led strategy which aimed to improve blood pressure and cholesterol management in PLWH. The trial demonstrated that coordinated care and patient education could effectively lead to better cardiovascular outcomes, highlighting the potential of personalized care in managing chronic conditions.
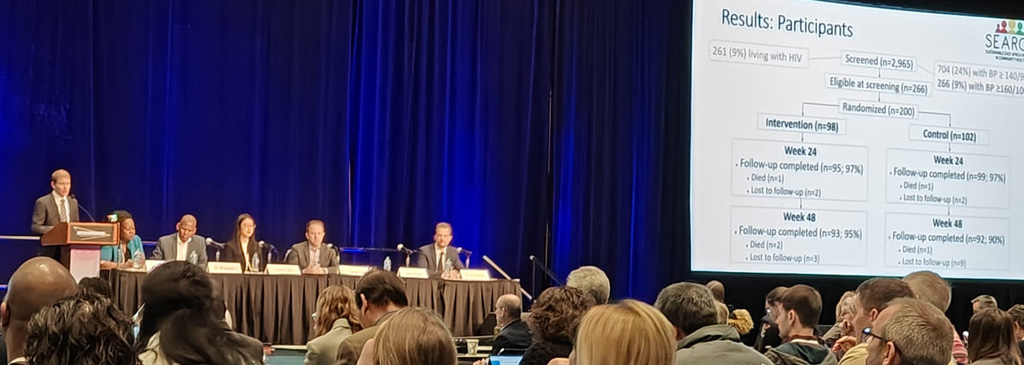
From the University of California San Francisco and the SEARCH research consortium, Matt Hickey (who also works with the HLB-SIMPLe RCC) shared findings from a study conducted in rural Kenya and Uganda. The research tested a telehealth approach for managing severe hypertension facilitated by community health workers. They found that the approach improved blood pressure control and care retention among the 200 participants, demonstrating that telehealth interventions focused on individuals with severe hypertension is a high-yield approach to improve outcomes among those with highest risk for cardiovascular disease.
Another significant revelation came from the REPRIEVE trial, presented by Márton Kolossváry from Massachusetts General Hospital. The study showed that Pitavastatin significantly reduces non-calcified plaque in PLWH, independent of cholesterol levels. The study suggested that the medication’s effect might be mediated by a protein involved in collagen formation, opening new possibilities for cardiovascular disease treatment in HIV patients. Kristine M Erlandson from the University of Colorado Anschutz Medical Campus presented other REPRIEVE findings assessing the impact of Pitavastatin on physical function in PLWH. This research, which included 602 participants over five years, found no significant difference in physical function decline between those taking the statin and those on placebo. These findings provide critical insights into the long-term use of statins in HIV patients.
Finally, Nomathemba Chandiwana from the iHEART-SA project presented on another study she worked on in South Africa, which looked at how a certain type of HIV treatment called dolutegravir-based therapy might affect weight gain when combined with diet and activity. The research team followed a group of people for 48 weeks to see how their weight changed while on this treatment. The findings suggest that while some people did gain weight, it wasn’t significant overall, and factors like diet and physical activity seemed to play a role. This suggests that while dolutegravir-based therapy might be associated with weight gain in some cases, lifestyle factors also matter.
The conference demonstrated a significant evolution in understanding HIV and its intersections with noncommunicable diseases. The presented studies highlight the importance of developing holistic treatment approaches for PLWH, addressing not just the virus but also the broader health challenges they face. This year’s conference reaffirmed the scientific community’s commitment to advancing HIV research in conjunction with broader health concerns, ensuring a more comprehensive care approach for those living with HIV.
HLB-SIMPLe is funded by the Center for Translation Research and Implementation Science at the National Heart, Lung, and Blood Institute (NHLBI) and the Fogarty International Center at the US National Institutes of Health (NIH) through grants U24-HL-154426, UH3-HL154499, UH3-HL-156390, UH3-HL-154498, UH3-HL-156388, UH3-HL-154501, UH3-HL-156389.